Don’t feel rested when you wake up? You may need a sleep test
Despite having a long night, more than 6 hours of sleep, you still feel very sleepy or fatigue during the day. This may be a sign that your sleep quality may not be as good as it should be. Moreover, your partner keeps complaining about how you snore so loud and regularly. If this seems familiar to you, you should start thinking that you may have obstructive sleep apnea.
Obstructive sleep apnea (OSA) is a highly prevalent disease. It affects people ranged from 9% to 38% in the general adult population and can be found as high as 30% of men who are older than 40 years.(1) However, the disease has been underrated and underdiagnosed since more than 80% may not seek medical attention.(2) Untreated OSA not only cause chronic sleepiness which impairs your quality of life, affects your daytime function and mood but also can lead to undesirable long term cardiovascular diseases such as hypertension, diabetes, stroke, and heart attack.(3)
The hallmark symptom of OSA is snoring. Snoring happens when your throat muscles collapse and pharyngeal space becomes significantly narrow due to loss of tone during sleep. Due to its commonness, it’s often overlooked. Nevertheless, people who habitually snore (>3 night/week) or snore loudly (louder than normal talking) may be at risk of having sleep disordered breathing.(4)
How do we know if we have sleep apnea?
You may be at increased risk of having OSA if you have the following symptoms(5):
- Habitual or loud snoring
- Daytime sleepiness, feeling low energetic or fatigue
- Obesity or you carry more weight than is healthy for you
- Age older than 50
- High blood pressure, atrial fibrillation, stroke or coronary heart disease
Sleep studies for OSA
A sleep study can help us find out if you have sleep apnea. It provides detailed information about your sleep, breathing, heart rate and other biosignals during sleep. It is recommended by the American Academy of Sleep Medicine that you should get the test done before getting treatment.(6) Not only to confirm the diagnosis, but also it can help identify the severity of the disease, and potential modality of treatment.
Depending on how bad your symptoms are and your clinical circumstance, we’ll recommend either an in-lab sleep study at the hospital or one that you can do by yourself at home.
- Overnight sleep study (polysomnography): You’ll spend the night in a comfortable, private room. While you sleep, the sleep technologist will measure your breathing patterns, brain activity and eye movements.
- Home Sleep Apnea Test (HSAT): We’ll give you a sleep monitoring device and instructions on how to use it. You’ll use the device as you sleep, just for one night. While you sleep in the comfort of your home, the device records any breathing disturbances.
After your sleep study, our providers will go over the results with you and tell you if you have obstructive sleep apnea.
Why should you get a sleep consultation at RPH?
- There is a sleep specialist at Royal Phnom Penh Hospital who has been board certified by World Sleep Society, a well renowned sleep medicine international organization. We’ll make sure that you get a high quality, standardized care by an expertise qualified in the field.
- Royal Phnom Penh Hospital is one of the top (if not only) healthcare institutes in Cambodia that can provide you a variety of sleep study services using the high quality software and devices approved by the FDA-US, or FDA-Thai.
- Royal Phnom Penh Hospital is a trusted healthcare leader in Cambodia. We're recognized in the national and international level and we’re the only one hospital that received JCI accreditation in the country.
- If you have any other health problems that also need attention, your care team includes not only experts in sleep medicine but also specialists in associated fields including neurologist, cardiologist, internist, psychologist, etc. We’ll work together to get the right diagnosis and the best treatment plan for you.
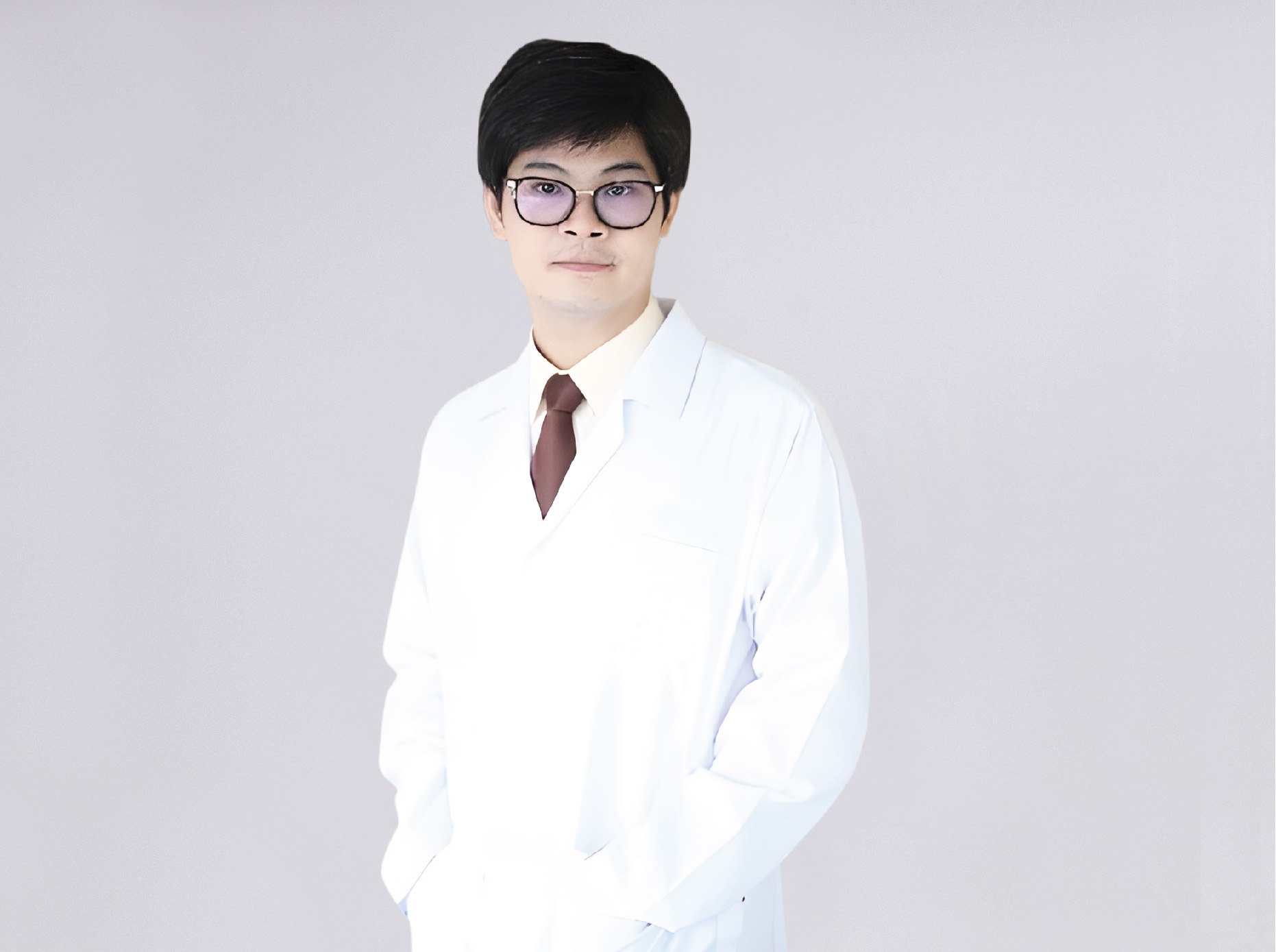
Dr. Somprasong Liamsombut
Internist/ Pulmonary And Critical Care Medicine/ Sleep Medicine
References:
- Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev. 2017 Aug;34:70-81
- Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ. 2009 Aug;108(5):246-9
- Veasey SC, Rosen IM. Obstructive Sleep Apnea in Adults. N Engl J Med. 2019 Apr 11;380(15):1442-1449
- Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108: 768–75
- Chiu HY, Chen PY, Chuang LP, Chen NH, Tu YK, Hsieh YJ, Wang YC, Guilleminault C. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: A bivariate meta-analysis. Sleep Med Rev. 2017 Dec;36:57-70
- Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017 Mar 15;13(3):479-504






